The giant pharmaceutical company, Bristol-Myers Squibb, faced two law suits for alleged misrepresentation of its blood thinner products, Eliquis and Plavix. Eliquis is an anticoagulant used to prevent blood thinner stroke. Plavix is an antiplatelet used to protect patients from stroke and heart diseases. The two lawsuits against Bristol-Myers Squibb are vital in enhancing the understanding of blood thinner stroke.
In 2017, Carmen Flores filed a lawsuit against Bristol-Myers Squibb, arguing that she developed an ischemic stroke while on Eliquis prescription. Flores argued that Eliquis led her to experience excessive bleeding, which disrupted her blood supply to the brain. She became prone to ischemic stroke. Flores told the courts that Bristol-Myer used its strength in treating cardiovascular diseases to commercialize Eliquis. However, the company failed to demonstrate Eliquis as a possible cause for blood thinner stroke. In its ruling, the court explained the need for pharmaceutical companies to provide truthful information to consumers.
In a similar lawsuit, Bristol-Myers is facing another blood thinner lawsuit for its product, Plavix. The plaintiff argues that the manufacturer promoted the product as beneficial to cardiovascular patients. The manufacturer further stated that Plavix is safer and easier on a patient’s stomach than aspirin. The ruling on the case is yet to be made, but patients argue that Plavix causes stroke and excessive bleeding.
The two lawsuits above require assessing the relationship between blood thinner and stroke. It helps review expert opinion on whether non-valvar atrial fibrillation patients risk stroke since they take blood thinners. It further helps assess the best blood thinner after stroke for patients at risk of blood clotting.
Can too much blood thinner cause stroke?
One of the known side effects emerging from the consumption of too many blood thinners is stroke. Doctors prescribe blood thinners to patients with an increased risk of blood clotting, such as non-valvar atrial fibrillation. Blood clots can be life-threatening if they disrupt the regular blood supply in all body parts. Hence, blood thinners have a medical value for some people. However, stroke is the third leading cause of death for both men and women. Evaluating whether blood thinners cause stroke will be critical in reducing the mortality rate.
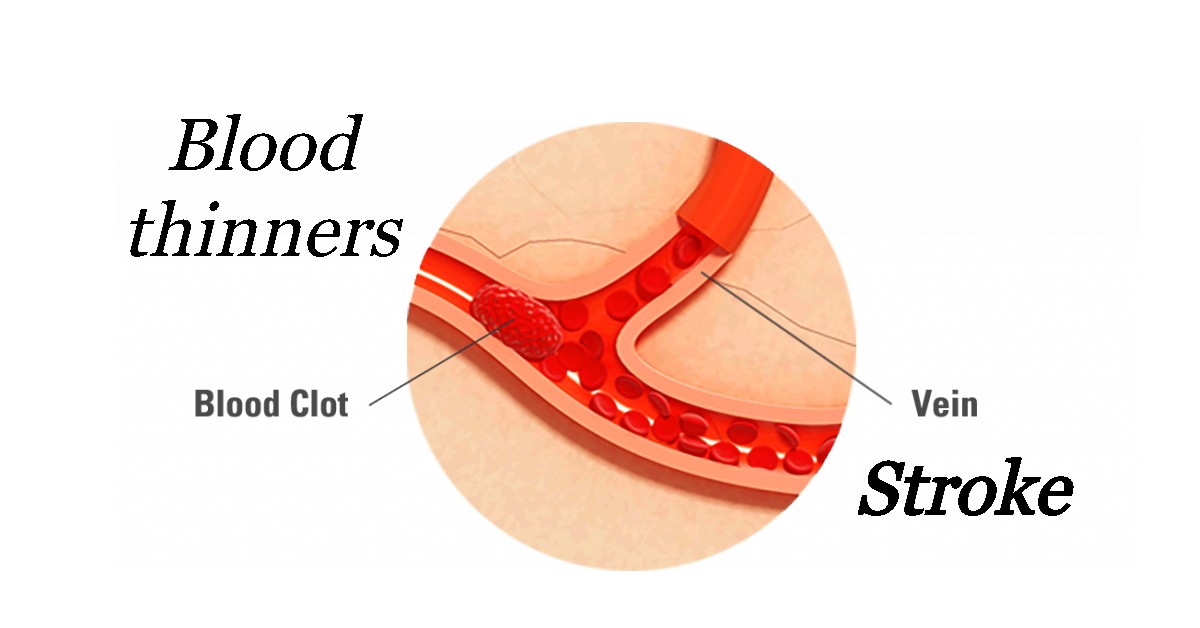
Blood thinner stroke emerges from unregulated blood pressure and clot formations. A stroke is a medical condition that arises after disrupting the blood supply to a particular brain part. There are two types of stroke, ischemic and hemorrhagic, depending on how they occur.
Ischemic and hemorrhagic stroke
Ischemic stroke occurs when a clot in arteries inhibits blood supply. Patients with atrial fibrillation and heart diseases have a high risk of suffering from ischemic stroke. A hemorrhagic stroke happens after a rupture or leakage of a blood vessel. Individuals who overuse blood thinners are at a higher risk of suffering from a hemorrhagic stroke. Blood vessels located beyond the area of rupture experience a reduced blood supply.
Healthcare givers seek to identify whether a patient suffers from ischemic or hemorrhagic stroke. There is a complex relationship between blood thinners and stroke. Blood thinners play an essential role in treating ischemic stroke.
However, using blood thinners for hemorrhagic stroke patients aggregates the bleeding. Individuals consuming blood thinners and at high risk of stroke should look for symptoms associated with the disease. Ischemic stroke also causes hemorrhagic stroke when it causes a vessel rapture. These symptoms include paralysis of muscles, slurred speech, vomiting, dizziness, severe headache, and reduced consciousness.
Blood thinner as a stroke prevention
Blood thinner and stroke have a positive relationship because both anticoagulants and antiplatelets can help prevent the disease. Doctors prescribe blood thinners to the patient suffering from ischemic stroke. Health experts prescribe blood thinners to help prevent patients at risk of ischemic stroke before it strikes. In other instances, doctors prescribe blood thinners after a patient experiences a transient stroke to prevent a recurrence. Patients with heart diseases and atrial fibrillation take a blood thinner to lower the risk of stroke.
Blood clotting is an essential process of the body because it stops bleeding and prevents infections. However, blood clots pose a health risk if they can travel to the brain and disrupt blood flow. Blood thinner stroke is the probable health implication of consuming too many anticoagulants and antiplatelets. Despite the risks associated with blood thinner and stroke, some individuals must take the medication due to underlying health conditions.
Antiplatelet is among the medication used to treat ischemic blood thinner stroke. Platelets refer to the blood cells that create blood clots. Patients at the risk of a stroke attack take antiplatelet medication to make platelets less sticky. Platelets are unlikely to form clots when they are not sticky. Doctors also prescribe antiplatelet medicine to prevent a recurrence of a stroke attack. Patients must adhere to prescriptions given to avoid other risks associated with blood thinners. Aspirin and Plavix are the blood thinners used to protect patients against stroke attacks.
Doctors also prescribe anticoagulants to patients at risk of a stroke attack. Anticoagulants help to reduce the chances of blood-forming clots. The medication is powerful in blood thinning, and experts advise patients to follow the prescribed dose strictly. Patients taking anticoagulants undergo frequent blood tests to assess their risk of contracting blood thinner stroke. The common anticoagulants used to prevent stroke are heparin and warfarin. Healthcare givers use heparin for short-term goals in the hospital. Warfarin is slow acting and recommended for long-term use among patients at risk of blood clotting.
Research in the healthcare sector led to the identification of several other blood thinners recommended for patients at risk of clot formation. Such new medications include Pradaxa, Elequis, Xarelto, and Savaysa. The new blood thinner stroke medicine is slower acting than warfarin. Patients can use it for the long term without requiring frequent blood tests. The new medication has a lower rate of excessive bleeding than other drugs associated with blood thinner and stroke.
Blood thinner for stroke risk
Doctors prescribe blood thinners to minimize the risk of stroke among patients suffering from clot formation and heart diseases. Non-valvar atrial fibrillation makes the most significant portion of blood thinner consumers. Blood thinners reduce the disruption of the blood supply into the brain since the platelets are less sticky.
However, patients at the risk of blood thinner stroke must strictly adhere to the prescription given to avoid any severe implications. Patients taking blood thinners to protect themselves from suffering a stroke must make some lifestyle adjustments. Examples of recommended lifestyle adjustments should help reduce the risk of getting injured, prompting bleeding. Blood thinners help prevent clot formation and thin blood leading to a risk of excessive bleeding. The negative implication is more severe for some people compared to others. Taking blood thinner to reduce the risk of stroke is therefore not viable for some people due to underlying health conditions.
Best blood thinner after stroke
Doctors prescribe blood thinners to patients after a stroke attack as a preventive measure to inhibitrecurring strokes. Ischemic stroke results from the formation of clots in the arteries, which disrupt the blood supply to the brain. Taking blood thinners minimizes the chances of clot formation for the consumers. Stroke patients must identify the actual cause of the attack to determine the best blood thinner after stroke. Failure to identify the cause can harm a patient’s condition if one suffers a hemorrhagic stroke.
Antiplatelet medication is the best blood thinner after stroke because it helps reduce the chances of clot recurrence in arteries. The commonly used antiplatelets include aspirin and Plavix. Aspirin is the most popular antiplatelet since it has been in existence longer than other blood thinners. It has been the best blood thinner after stroke. However, aspirin has some severe side effects for the patients, including stomach upset. Patients should constantly discuss their response to medicine with their doctors. Doctors can use the feedback to recommend other medicinal alternatives for the best blood thinner after stroke. Other FDA-approved antiplatelet drugs in the pharmaceutical market include clopidogrel, prasugrel, ticlopidine, and ticagrelor.
Even though antiplatelet drugs are the best blood thinner after stroke, patients should only use the medicine under a doctor’s prescription. The medication has the capability of thinning blood, which can have negative implications such as excessive bleeding. Anticoagulants are not the best blood thinner after stroke because they help reduce the formation of clots. That means clot formation is possible but at a lowered rate. Patients who suffer ischemic stroke demonstrate that they are at a higher risk of clot formation. The effort made by the healthcare givers should be to eliminate clot formation to avoid a recurring attack.
Antiplatelet, as the best blood thinner after stroke, requires that patients undergo regular blood tests. The blood tests help determine the blood-thinning effect of the medication on the patient. While some patients must take blood thinners regularly, monitoring and making alternative suggestions are essential.
Healthcare givers are responsible for creating a lot of awareness for patients dealing with blood thinners and stroke. The literary health education should focus on lifestyle choices stroke patients make to improve their quality of life. Stroke patients should be made to understand their limits with blood thinners.
You can also check our hematicfood youtube channel, if you are interested to find out how food affects our blood condition.